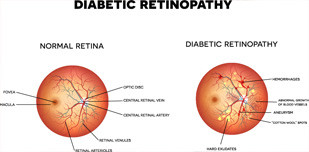
Diabetes (both Type I and Type II) can lead to a multitude of complications, including often forgotten eye-related complications, which are significant. One of the main ways in which diabetes can affect the eyes is diabetic retinopathy. This condition includes all manners of retinal disorders related to diabetes. The retina – the light-sensitive inner lining at the back of the eye – begins to deteriorate as the fine network of blood vessels is damaged leading to scarring of the retinal tissue, blocked vessels, growth of new fragile vessels, leaks, and swelling. Eventually these begin to impair vision.
It should be noted that in general, the term used to encompass all retinal conditions related to diabetes is 'diabetic retinopathy'. However, diabetic conditions specifically affecting the macula – the central part of the retina, which is responsible for sharp vision – are officially referred to as 'diabetic maculopathy'. Diabetic maculopathy can be divided into the subtypes of oedematous (accumulation of fluids and exudates in the macular region) and ischaemic (occlusion of macular blood vessels).
Worryingly, early changes in the retinal functioning may not cause noticeable symptoms for the patient. Due to this, it is imperative that anyone diagnosed with either type of diabetes have regular eye checks (yearly usually) to detect and diagnose changes at the earliest possible stage and initiate treatment when appropriate. Once the symptoms appear, they include blurred vision, sudden loss of vision, floaters in your vision, or missing/dark patches on images.
Diabetic retinopathy is a progressive condition, which can be broadly classified into the following stages:
There are two main triggers for vision loss in this condition; macular oedema and neovascularization. Macular oedema occurs when fluid and blood leaks from microaneurysms in the network of vessels. These leaks can cause swelling in the macula, which is responsible for sharp and colour vision. Neovascularization occurs when signals are sent from the retina to start growing new blood vessels to replace damaged vessels. Unfortunately, these new vessels are very fragile and have thin walls, which can leak blood and cause severe vision loss as well as lead to scarring that can pull the retina away from the back of your eye.

Anyone with either type of diabetes is at risk of developing diabetic retinopathy. The severity or progression of the condition can vary from one diabetic to the next, but the longer you are diabetic, the higher the risk becomes. High blood pressure and elevated cholesterol levels can exacerbate the condition, so beware and make sure your eyes are checked regularly. If you are diabetic and are or become pregnant, you should have a comprehensive dilated ophthalmological examination as soon as possible and follow the guidelines and possible further evaluations recommended by your ophthalmologist.
Diagnosis can be done only by an ophthalmologist during a complete ophthalmological examination. Finland Eye Center offers a 'Diabetic Retinopathy Assessment Package', which includes the following:
Finland Eye Center is equipped with a fully functioning laboratory for all laboratory investigations including blood sugar level tests.
Strict control of blood sugar, blood pressure and blood cholesterol – to reduce the risk factors – is essential. Depending on the severity and progressional trajectory of your diabetic retinopathy, several options are available at Finland Eye Center to manage the condition.
Your ophthalmologist will inform and advise you of the best option (or combination of options) for your situation. It is important to understand that treatment may need to be repeated and that curing the condition is not possible as the risk of new bleeding always exists since diabetes is a chronic disease.